Post by Admin on Oct 14, 2020 21:52:00 GMT
UNDERSTANDING AGE-ADJUSTED MORTALITY RATES
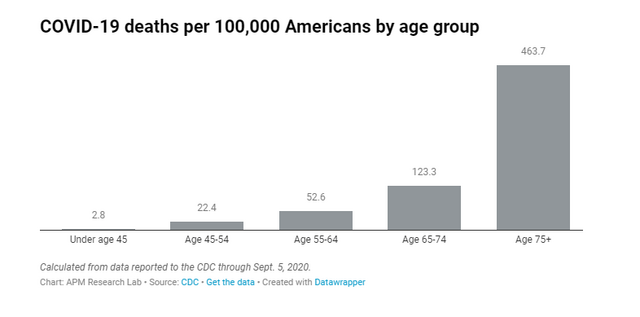
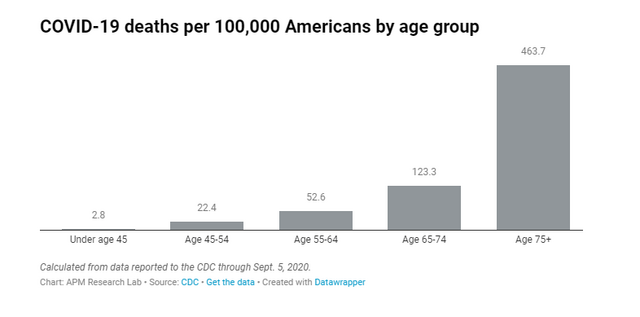
While there are many features of the novel coronavirus that are still unclear, this we know with certainty: The risk of dying from COVID-19 rises sharply with advanced age. About 3 in 100,000 Americans under age 45 have died from the virus, according to data submitted to the CDC through Sept. 5. The COVID-19 death rate for Americans age 45-54 rises to 22 per 100,000; more than doubles for those age 55-64 (53 per 100,000); and more than doubles among those age 65-74 (123 per 100,000). Among Americans age 75 and older, the death toll is exceedingly high: 464 people per 100,000, as shown below.
Due to this steep age gradient to COVID-19 mortality, it is important to consider the varying age distributions of America’s racial and ethnic groups. A higher share of White Americans are in the older age brackets than any other group. To illustrate this, consider that the median age of non-Hispanic White Americans is 44 years, according to the latest Census Bureau data. The comparable figure for all populations of color is considerably lower—for Asians (37), Blacks (34), Pacific Islanders (33), Indigenous (32) and especially Latinos (30), half of whom have not yet reached their 30th birthday.
Even within the same race groups, the age distribution varies—with retirement destination states such as Florida having a much higher share of older adults within their White population, for example.
Black, Indigenous, Pacific Islander and Latino Americans all have a COVID-19 death rate of roughly triple or more White Americans (age-adjusted).
So, to remove the role of age differences from COVID-19 mortality rates, we have also produced age-adjusted rates. Because mortality data is not available for all states by race and age jointly (which is preferred), we have used indirect standardization to calculate these rates. See our NOTES section for details and cautions about our method.
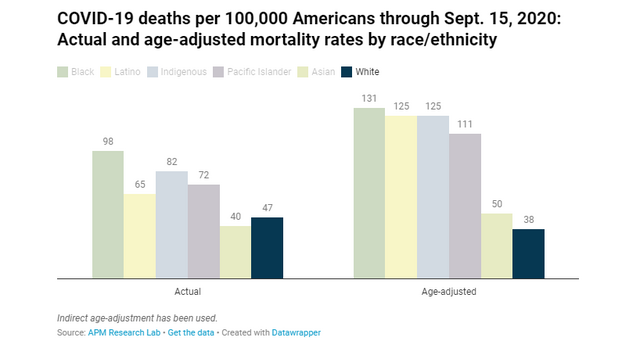
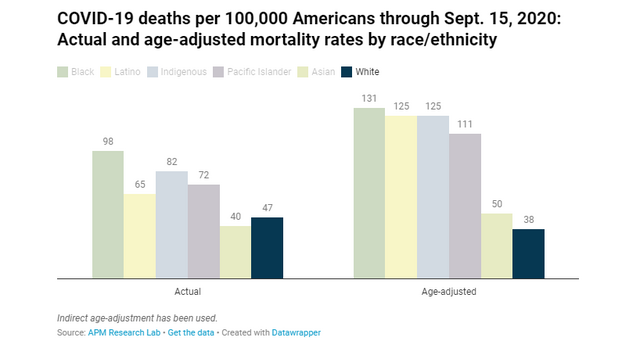
Adjusting the racial data we’ve collected for age differences increases the COVID-19 mortality rate for all racial and ethnic groups except for Whites, who experience a decrease, as shown below. Latinos’ rate rises the most following age-adjustment, revealing that the virus is impacting Latinos far more than would be expected based on their age profile.
While Black Americans continue to experience the highest COVID-19 mortality rate after age-adjusting, doing so also widens the gap between Black and White mortality—from 2.2 to 3.4 times as high. Mortality rates for Indigenous people rise to 3.3 times as high as Whites’ mortality impact. Rates for Latinos and Pacific Islanders also rise substantially, to 3.3 and 2.9 times as high as Whites, respectively. Finally, the Asian mortality rate—which was slightly below the White rate—rises above the White death rate (1.3 times as high), when age is taken into account. Put another way, Black, Indigenous, Pacific Islander and Latino Americans all have COVID-19 death rates of roughly triple or more the rate of White Americans (age-adjusted).
What does this mean? It indicates that many younger Americans who are Black, Latino, Indigenous or Pacific Islanders are dying of COVID-19—driving their mortality rates far above White Americans’. Despite their relative youthfulness (a protective factor against COVID), their death rates are elevated. As Brookings Institution has reported, “In every age category, Black people are dying from COVID at roughly the same rate as White people more than a decade older.”
Depending on the community, this may be due to numerous, reinforcing factors related to a higher likelihood of contracting the virus—such as greater workplace exposures, including inability to work from home or no access to sick days; living in geographic areas, housing arrangements including congregate settings (such as nursing homes, group homes, treatment centers, correctional facilities), or accessing public transportation where the virus is more easily spread. It also results from poorer outcomes after acquiring COVID-19—such as resulting from less access to testing; higher presence of underlying health conditions like diabetes, hypertension, obesity and asthma; and receiving delayed or poorer medical care, perhaps because they lack health insurance or distrust health providers or they are simply receiving inferior care. The racial disparities in COVID-19 mortality—due to these compounding, elevated risks from our systems of housing, labor force, health care, and policy responses—are the result of systemic racism.
It is important to note that, while age-adjusted mortality rates help us remove the influence of age differences in racial groups to examine disparities in outcomes, they are not the actual mortality rates experienced by these groups.
While there are many features of the novel coronavirus that are still unclear, this we know with certainty: The risk of dying from COVID-19 rises sharply with advanced age. About 3 in 100,000 Americans under age 45 have died from the virus, according to data submitted to the CDC through Sept. 5. The COVID-19 death rate for Americans age 45-54 rises to 22 per 100,000; more than doubles for those age 55-64 (53 per 100,000); and more than doubles among those age 65-74 (123 per 100,000). Among Americans age 75 and older, the death toll is exceedingly high: 464 people per 100,000, as shown below.
Due to this steep age gradient to COVID-19 mortality, it is important to consider the varying age distributions of America’s racial and ethnic groups. A higher share of White Americans are in the older age brackets than any other group. To illustrate this, consider that the median age of non-Hispanic White Americans is 44 years, according to the latest Census Bureau data. The comparable figure for all populations of color is considerably lower—for Asians (37), Blacks (34), Pacific Islanders (33), Indigenous (32) and especially Latinos (30), half of whom have not yet reached their 30th birthday.
Even within the same race groups, the age distribution varies—with retirement destination states such as Florida having a much higher share of older adults within their White population, for example.
Black, Indigenous, Pacific Islander and Latino Americans all have a COVID-19 death rate of roughly triple or more White Americans (age-adjusted).
So, to remove the role of age differences from COVID-19 mortality rates, we have also produced age-adjusted rates. Because mortality data is not available for all states by race and age jointly (which is preferred), we have used indirect standardization to calculate these rates. See our NOTES section for details and cautions about our method.
Adjusting the racial data we’ve collected for age differences increases the COVID-19 mortality rate for all racial and ethnic groups except for Whites, who experience a decrease, as shown below. Latinos’ rate rises the most following age-adjustment, revealing that the virus is impacting Latinos far more than would be expected based on their age profile.
While Black Americans continue to experience the highest COVID-19 mortality rate after age-adjusting, doing so also widens the gap between Black and White mortality—from 2.2 to 3.4 times as high. Mortality rates for Indigenous people rise to 3.3 times as high as Whites’ mortality impact. Rates for Latinos and Pacific Islanders also rise substantially, to 3.3 and 2.9 times as high as Whites, respectively. Finally, the Asian mortality rate—which was slightly below the White rate—rises above the White death rate (1.3 times as high), when age is taken into account. Put another way, Black, Indigenous, Pacific Islander and Latino Americans all have COVID-19 death rates of roughly triple or more the rate of White Americans (age-adjusted).
What does this mean? It indicates that many younger Americans who are Black, Latino, Indigenous or Pacific Islanders are dying of COVID-19—driving their mortality rates far above White Americans’. Despite their relative youthfulness (a protective factor against COVID), their death rates are elevated. As Brookings Institution has reported, “In every age category, Black people are dying from COVID at roughly the same rate as White people more than a decade older.”
Depending on the community, this may be due to numerous, reinforcing factors related to a higher likelihood of contracting the virus—such as greater workplace exposures, including inability to work from home or no access to sick days; living in geographic areas, housing arrangements including congregate settings (such as nursing homes, group homes, treatment centers, correctional facilities), or accessing public transportation where the virus is more easily spread. It also results from poorer outcomes after acquiring COVID-19—such as resulting from less access to testing; higher presence of underlying health conditions like diabetes, hypertension, obesity and asthma; and receiving delayed or poorer medical care, perhaps because they lack health insurance or distrust health providers or they are simply receiving inferior care. The racial disparities in COVID-19 mortality—due to these compounding, elevated risks from our systems of housing, labor force, health care, and policy responses—are the result of systemic racism.
It is important to note that, while age-adjusted mortality rates help us remove the influence of age differences in racial groups to examine disparities in outcomes, they are not the actual mortality rates experienced by these groups.


